Ringworm, Athletes foot and Jock itch
What Is Tinea?
Tinea (or
Tinea or ringworm is a usually mild skin infection with a fungus, so it is not caused by a worm (see picture at WebMD! (Citations 1, 2) The ringworm name comes from the ring-shaped red spots that develop on the skin. Another medical term for tinea is
Dermatophytes are a group of three sub-families of fungi: Trichophyton,
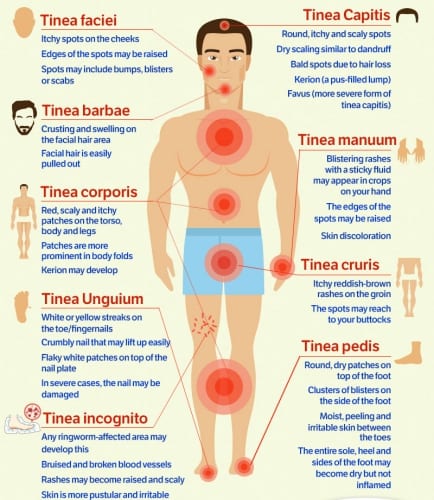
The most common ones are ringworm of the scalp (tinea capitis), the feet (tinea pedis or athlete’s foot), the groin (tinea cruris or jock itch), the nails (tinea unguium or onychomycosis), or of other body surfaces (tinea corporis or ringworm of the body). (Citations: 4, 5) Less common ones are ringworm of the beard and mustache (
How common is Tinea?
Tinea is common in most countries and occurs more frequently in areas with poor hygiene. (Citation: 7) In a recent global burden of diseases study, fungal skin infections were the 4th most prevalent disease (Citation: 8), and dermatophytoses make up a significant portion of these. It is estimated that every 1 to 2 out of 10 persons will get a dermatophyte infection somewhere in life. (Citation: 9)
Is a Tinea infection contagious?
Tinea is contagious and is usually spread through direct contact with an infected person or animal (cat, dog, cattle, guinea-pig). It is also possible to get ringworm through contact with contaminated soil, contaminated surfaces (chairs, swimming pool floors etc.) or contaminated items (like toilet articles, clothing, chair, towel, bedclothes etc.). (Citation: 7) There are conditions and circumstances that increase the risk of getting tinea. They include impaired immunity, close contact with animals, use of public locker rooms and public showers, engagement in contact sports, warm and humid circumstances (tight shoes, hot/humid climates, excessive sweating) and poor hygiene. (Citation: 1)
What Are the Signs and Symptoms of Tinea?
The signs and symptoms vary a bit dependent on the area of the body that is infected. In general, there is itching and ring-shaped red areas that are scaling and/or cracked. In tinea of the scalp, beard etc. there might be hair loss. (Citation: 10)
Ringworm of the scalp (tinea capitis): Tinea capitis is most common in children of primary school age. This type of tinea can appear in many different forms. It often shows as several round spots of baldness, with or without inflammation. Especially non-inflamed areas might appear as “black dot ringworm”; the black dots are infected broken off hairs. The “gray type” of tinea capitis has round bald spots with a lot of scales. The “diffuse scale” type has a lot of scales all over the scalp, which might look a lot like dandruff. The ‘moth-eaten” type also has scales combined with patchy hair loss. More inflammation with often enlarged lymph nodes in the neck is seen in the “kerion” type and the “diffuse pustular pattern” type. The kerion refers to a localized swelling similar to an abscess while the diffuse pustular pattern relates to the extensive spread of pustules (pimples filled with pus). The last one is easily misdiagnosed as a bacterial infection, although there might also be a bacterial co-infection. In the “favus” type there are yellow crusts and matted hair. (Citations: 9, 11, 12, 13)
Athlete’s foot (tinea pedis): Tinea pedis usually affects the areas between the toes (the toe webs), particularly the between the 4th and 5th (little) toe. Commonly it shows a red cracked skin with flakes and itching. The skin might also become white and thicker with or without some swelling. When the infection spreads to the foot sole, this is called “moccasin athlete’s foot”. Athlete’s foot is related to warmth and sweating and occurs more often among people practicing certain sports (running, swimming) and in men and older people. (Citation: 14)
Jock itch (tinea cruris): Jock itch is found at the medial part of the upper thigh, in the groin area. The penis and scrotum are usually not involved. This
Onychomycosis (ringworm of the nails or tinea unguium): Ringworm affects more often the toenails than the fingernails and is more common in (older) adults. It has a relation with poor diabetic control and poor circulation, but also with too tight shoes and use of public locker rooms and showers. Onychomycosis can affect the nail itself, the nailbed or both. The nails become white or yellow and lose their normal shape. (Citations: 9,16)
Ringworm of the body (Tinea corporis): This form of tinea is more common in children and adults who live in humid, hot climates. It can occur anywhere on the body except for scalp, nails, groins, feet, hands, face (including beard and mustache areas). Pink to red round spots
How to diagnos a Tinea infection in humans?
Tinea infections are often recognized by doctors on their appearance. They can also be diagnosed by microscope examination of or laboratory testing of skin samples or scrapings. A culture is also possible to determine the type of Tinea infection present. The old method of using a Wood’s lamp to detect fluorescence of fungi only works for a few Microsporum fungus types. (Citations: 20, 21, 22, 23)
What Is the treatment for a Tinea infection?
The treatment for tinea usually consists of a topical application of a non-prescription antifungal cream, powder or lotion for 2-4 weeks, for example, Clotrimazole, Miconazole, Terbinafine or Ketoconazole. (Citation: 24) The most effective antifungal topical specifically for athlete’s foot is Terbinafine. (Citation: 25)
For tinea capitis (scalp ringworm) a longer treatment is needed (1-3 months) with oral prescription antifungals like Griseofulvin or Terbinafine, other options or itraconazole and fluconazole. (Citation: 26) For ringworm of the scalp topical application of antifungal medications is not sufficient. Often the oral treatment is combined with a topical application to speed up recovery and reduce the change of spreading the tinea to others. An easy topical application for the scalp is shampoo with selenium sulfide or ketoconazole as an ingredient. (Citation: 27)
Are there complications from Tinea infections in humans?
The most common problem with tinea infections is the spreading from one area to another, for example through scratching at different places of the body. In tinea capitis and tinea barbae, the complication is often hair loss and (patchy) baldness. Especially in people with broken skin and/or impaired immunity secondary bacterial infections might develop, but also in the pustular type of ringworm of the scalp. A rare problem is the development of scars, especially in the kerion type of tinea capitis. (Citation: 28) A topical application to the scalp can, however, be used to prevent the spread of the tinea capitis; this can also be a shampoo. (Citation: 29)
What are preventive measures against Tinea?
The most important preventive measure for tinea is good hygiene: regular washing with soap and
Scratching should be avoided to prevent spreading the infection to other parts of the body. People with athlete’s foot should for example wash, treat (topical application) and clothe their feet before they put on underwear. Athlete’s foot can also be prevented through wearing shoes that let the feet breathe and are not too tight and alternating shoes so as not to wear the same pair every day. (Citation: 14)
Other prevention measures are the treatment of your pets that have ringworm and keeping your nails short and clean. (Citation: 34)
References
- Centers for Disease Control and Prevention. Accessed online 14th September 2017. Weblink: https://www.cdc.gov/fungal/diseases/ringworm/health-professionals.html
- Web MD. Accessed online 14th September 2017. Weblink: http://www.webmd.com/skin-problems-and-treatments/picture-of-ringworm-of-the-body-tinea-corporis
- Merck Manual Professional Version. Accessed online 14th September 2017. Weblink: http://www.merckmanuals.com/professional/dermatologic-disorders/fungal-skin-infections/overview-of-dermatophytoses
- Accessed online 14th September. Weblink: https://www.uptodate.com/contents/dermatophyte-tinea-infections
- Merck Manual Professional Version. Accessed online 14th September 2017. Weblink: http://www.merckmanuals.com/professional/dermatologic-disorders/nail-disorders/onychomycosis
- DermNet New Zealand. Accessed online 14th September 2017. Weblink: https://www.dermnetnz.org/topics/tinea-faciei/
- World Health Organization. Accessed online 12th September 2017. Weblink: http://www.who.int/water_sanitation_health/diseases-risks/diseases/ringworm/en/
- Roderick J. Hay and others in “The Global Burden of Skin Disease in 2010: An Analysis of the Prevalence and Impact of Skin Conditions” in the Journal of Investigative Dermatology. June 2014, Volume 134, Issue 6, Pages 1527–1534. Weblink: http://www.jidonline.org/article/S0022-202X(15)36827-5/fulltext#s0020
- American Association of Family Practitioners. Accessed online 14th September 2017. Weblink: http://www.aafp.org/afp/1998/0701/p163.html
- Centers for Disease Control. Accessed online 12th September 2017. Weblink: http://www.hse.ie/eng/health/az/R/Ringworm/Complications-of-ringworm.html#collapse_6
- Fuller and others in “Diagnosis and management of scalp ringworm” in British Medical Journal 8 March 2003; 326 (7388): Page 539-541. Weblink: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1125423/
- DermNet New Zealand. Accessed online 14th September 2017. Weblink: https://www.dermnetnz.org/topics/tinea-capitis
- Merck Manual Professional Version. Accessed online 14th September 2017. Weblink: http://www.merckmanuals.com/professional/dermatologic-disorders/fungal-skin-infections/tinea-capitis
- PubMed Health. Accessed online 14th September 2017. Weblink: https://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0072733/
- Web MD. Accessed online 14th September 2017. Weblink: http://www.webmd.com/men/tc/jock-itch-topic-overview#1
- Merck Manual Professional Version. Accessed online 14th September 2017. Weblink: http://www.merckmanuals.com/professional/dermatologic-disorders/nail-disorders/onychomycosis
- Accessed online 14th September 2017. Weblink: http://emedicine.medscape.com/article/1105828-overview
- Merck Manual Professional Version. Accessed online 14th September 2017. Weblink: http://www.merckmanuals.com/professional/dermatologic-disorders/fungal-skin-infections/tinea-corporis
- Accessed online 14th September 2017. Weblink: http://emedicine.medscape.com/article/1091473-clinical
- Mayo Clinic. Accessed online 12th September 2017. Weblink: http://www.mayoclinic.org/diseases-conditions/athletes-foot/diagnosis-treatment/diagnosis/dxc-20235949
- Mayo Clinic. Accessed online 12th September 2017. Weblink: http://www.mayoclinic.org/diseases-conditions/ringworm-body/diagnosis-treatment/diagnosis/dxc-20232363
- Merck Manual Professional Version. Accessed online 12th September 2017. Weblink: http://www.merckmanuals.com/professional/dermatologic-disorders/fungal-skin-infections/tinea-cruris
- DermNet New Zealand. Accessed online 14th September 2017. Weblink: https://www.dermnetnz.org/topics/wood-lamp-skin-examination/
- Centers for Disease Control. Accessed online 12th September 2017. Weblink: https://www.cdc.gov/fungal/diseases/ringworm/treatment.html
- Cochrane Reviews. Accessed onine 14th September 2017. Weblink: http://www.cochrane.org/CD001434/SKIN_creams-lotions-and-gels-topical-treatments-fungal-infections-skin-and-nails-foot
- Mayo Clinic. Accessed online 14th September 2017. Weblink: http://www.mayoclinic.org/diseases-conditions/ringworm-scalp/diagnosis-treatment/treatment/txc-20261846
- American Association of Family Practitioners. Accessed online 14th September 2017. Weblink: http://www.aafp.org/afp/2014/1115/p702.html
- Ireland Health Service. Accessed online 12th September 2017. Weblink: http://www.hse.ie/eng/health/az/R/Ringworm/Complications-of-ringworm.html#collapse_6
- Merck Manual Professional Version. Accessed online 12th September 2017. Weblink: https://www.merckmanuals.com/professional/dermatologic-disorders/fungal-skin-infections/tinea-capitis
- Web MD. Accessed online 14th September 2017. Weblink: http://www.webmd.com/men/tc/jock-itch-topic-overview#2
- Mayo Clinic. Accessed online 12th September 2017. Weblink: http://www.mayoclinic.org/diseases-conditions/athletes-foot/manage/ptc-20236317
- National Health Service United Kingdom. Accessed online 14th September 2017. Weblink: http://www.nhs.uk/Conditions/Ringworm/Pages/Prevention.aspx
- The International Foundation for Dermatology. Accessed online on 14th September 2017. Weblink: http://www.ifd.org/protocols/tinea-capitis
- Centers for Disease Control and Prevention. Accessed online 14th September 2017. Weblink: https://www.cdc.gov/fungal/diseases/ringworm/risk-prevention.html
Watch Videos To Learn More

