Candida symptoms and treatment in humans
What Is a Candida infection?
Candidiasis is a fungal infection caused by one of the members of the sub-family Candida, (Citation: 1) most commonly Candida albicans. Candidiasis can be an invasive infection (with the fungus going into the bloodstream) or a local infection of the mucous membranes (of the mouth, throat, esophagus, glans penis, foreskin, vulva or vagina). It can also infect the nails. Oral candidiasis is often called “oral thrush” while vaginal candidiasis is often called “vaginal yeast infection” or “vaginal thrush”.
How common Is Candidiasis?
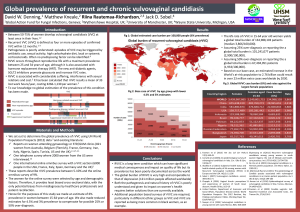
The most common form of candidiasis is the vulvovaginal type (infection of the vagina and its entry). It is estimated that 50-75% of women have a vulvovaginal Candida infection at least once in their life. A recurrent (at least 4 times in 1 year) vulvovaginal infection is estimated to take place in 6% of women of reproductive age (15-64 years), which means over 134 million women per year globally. (Citation: 2)
The non-genital forms of candidiasis are much less common and mostly occur in people with impaired immunity.
Is a Candida infection contagious?
Although people with a Candida infection are usually not contagious, people with impaired immunity might get the infection, as Candida can also live on the skin (Citations: 3, 11) While vaginal candidiasis is not considered to be a sexually transmitted disease, it can sometimes be transmitted to sexual partners.(Citation: 18) Especially with recurring vaginal candidiasis, it is important to also treat the sexual partner. (Citation: 4)
What are the signs and symptoms of Candidiasis?
The signs and symptoms of Candidiasis depend on the location and degree of the infection (invasive or not).
Vaginal candidiasis is characterized by itching and irritation of the vulva and vagina; pain or discomfort during sex and urination; and abnormal vaginal discharge. The vaginal discharge is often thick and white, with a cottage-cheese appearance. (Citations: 5, 6)
In oral thrush (Citation: 7), creamy white patches are seen on a red and sore background, often on the tongue and inner cheeks. Patients might have loss of taste and a cottony feeling in their mouth. They usually can have pain while eating and swallowing. (Citation: 8, 9)
People with invasive candidiasis can be quite sick including fever and chills. They often have other medical conditions that impaired their immunity (e.g. HIV, cancer, uncontrolled diabetes). Some patients also might have been treated with antibiotics for a suspected bacterial infection.(Citation: 10)
How is the diagnosis of Candidiasis made?
The diagnosis of candidiasis depends on the location of the infection.
A blood culture is done for invasive candidiasis. (Citation: 11) The diagnosis of vulvovaginal Candida infection is usually a combination of the symptoms and a simple examination of the vaginal discharge under the microscope. A culture of a vaginal smear is optional. (Citation: 12)
Oral thrush can often be diagnosed by a clinical examination – the diagnosis can be confirmed with an examination of a sample from mouth or throat. (Citation: 13)
What is the treatment for Candidiasis?
Treatment of Candidiasis depends on the location of the infection.
For candidiasis of the mouth and throat antifungal medication like Clotrimazole, Miconazole and Nystatin are used for a period of 7-14 days. They are applied to the inside of the mouth. (Citation: 14) For more severe infection of the mouth and throat and infections of the esophagus, Fluconazole is used (orally or intravenously). (Citation: 4)
For vulvovaginal candidiasis, WHO recommends treatment with an imidazole (Citation: 15), for example, Clotrimazole 500 mg intravaginal (single dose) or Miconazole or Clotrimazole 200 mg intravaginal daily for 3 days. The last one is one of the recommended options during pregnancy (Citation: 16).
For balanoposthitis (infection of the glans penis and foreskin) nystatin or Clotrimazole cream is applied twice daily for 7 days (Citation: 17).
Invasive candidiasis is usually treated intravenously with for example an echinocandin or fluconazole. (Citation: 18)
Are there complications from Candidiasis in humans?
The complications of candidiasis infections depend on their respective locations.
Complications of oral and vaginal thrush usually only occur in people with impaired immunity. They include the development of invasive Candida infection and/or the bacterial co-infection of the oral thrush lesions. (Citations: 19, 20)
Invasive candidiasis can affect heart, brain, bones, eyes and other body parts. (Citation: 21)
What are preventive measures against Candidiasis?
Prevention of candidiasis should take into account the risk factors. For example, the risk of developing a vaginal thrush is increased in people who use antibiotics, have uncontrolled diabetes, have high estrogen levels (pregnant women, high-dose estrogen oral contraceptive pills, estrogen hormone therapy), have an impaired immune system or have unprotected sexual contact (Citation: 22). Therefore, measures that might prevent (vaginal) yeast infections are a balanced diet, good control of blood sugar in diabetes patients and only using antibiotics if necessary. (Citation: 23) Also wearing of (loose) cotton underwear might help prevent vaginal thrush. (Citation: 24) High-risk patients for (invasive or other) candidiasis with impaired immunity often get antifungal prophylaxis and should pay special attention to hygiene. (Citation: 25)
Oral thrush can be prevented through good oral health, including cleaning of the mouth after use of inhalers with corticosteroids (Citation: 26).
References
- Centers for Disease Control. Accessed online 9th September 2017. Weblink: https://www.cdc.gov/fungal/diseases/candidiasis/
- Denning and others in: Global prevalence of recurrent and chronic vulvovaginal candidiasis. Accessed online 9th September 2017. Weblink: https://www.escmid.org/escmid_publications/escmid_elibrary/material/?mid=16168
- Medline Plus. Accessed online 9th September 2017. Weblink: https://medlineplus.gov/ency/article/000880.htm
- Ontario Government. Accessed online 9th September 2017. Weblink: http://www.health.gov.on.ca/en/public/publications/std/cand.aspx
- Mayo clinic. Accessed online 9th September 2017. Weblink: http://www.mayoclinic.org/diseases-conditions/yeast-infection/basics/symptoms/con-20035129
- Centers for Disease Control. Accessed online 9th September 2017. Weblink: https://www.cdc.gov/fungal/diseases/candidiasis/genital/index.html
- Centers for Disease Control. Accessed online 9th September 2017. Picture of oral thrush. Weblink: https://phil.cdc.gov/phil/details.asp?pid=1217
- Mayo clinic. Accessed online 9th September 2017. Weblink: http://www.mayoclinic.org/diseases-conditions/oral-thrush/home/ovc-20342105
- Centers for Disease Control. Accessed online 9th September 2017. Weblink: https://www.cdc.gov/fungal/diseases/candidiasis/thrush/index.html
- Centers for Disease Control. Accessed online 9th September 2017. Weblink: https://www.cdc.gov/fungal/diseases/candidiasis/invasive/symptoms.html
- Centers for Disease Control. Accessed online 9th September 2017. Weblink: https://www.cdc.gov/fungal/diseases/candidiasis/invasive/diagnosis.html
- Centers for Disease Control. Accessed online 9th September 2017. Weblink: https://www.cdc.gov/fungal/diseases/candidiasis/genital/index.html
- Centers for Disease Control. Accessed online 9th September 2017. Weblink: https://www.cdc.gov/fungal/diseases/candidiasis/thrush/index.html
- Centers for Disease Control. Accessed online 9th September 2017. Weblink: https://www.cdc.gov/fungal/diseases/candidiasis/thrush/index.html
- World Health Organization. Accessed online 9th September 2017. Weblink: http://apps.who.int/medicinedocs/es/d/Jh2942e/4.11.1.html
- World Health Organization. Accessed online 9th September 2017. Weblink: http://apps.who.int/medicinedocs/es/d/Jh2942e/4.11.2.html
- World Health Organization. Accessed online 9th September 2017. Weblink: http://apps.who.int/medicinedocs/es/d/Jh2942e/4.11.4.html
- Centers for Disease Control. Accessed online 9th September 2017. Weblink: https://www.cdc.gov/fungal/diseases/candidiasis/invasive/treatment.html
- Mayo Clinic. Accessed online 9th September 2017. Weblink: https://www.mayoclinic.org/diseases-conditions/oral-thrush/symptoms-causes/dxc-20342110
- Morales and others in Candida albicans Interactions with Bacteria in the Context of Human Health and Disease. PLoS Pathog. 2010 Apr; 6(4): e1000886. Published online 2010 Apr 29. doi: 1371/journal.ppat.1000886. PMCID: PMC2861711. Weblink: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2861711/
- Mayo Clinic. Accessed online 9th September 2017. Weblink: https://www.cdc.gov/fungal/diseases/candidiasis/invasive/index.html
- Mayo Clinic. Accessed online 9th September 2017. Weblink: https://www.mayoclinic.org/diseases-conditions/yeast-infection/basics/risk-factors/con-20035129
- Accessed online 9th September 2017. Weblink: https://www.webmd.com/women/tc/vaginal-yeast-infections-prevention
- Centers for Disease Control. Accessed online 9th September 2017. Weblink: https://www.cdc.gov/fungal/diseases/candidiasis/genital/index.html
- Centers for Disease Control. Accessed online 9th September 2017. Weblink: https://www.cdc.gov/fungal/diseases/candidiasis/invasive/risk-prevention.html
- Centers for Disease Control. Accessed online 9th September 2017. Weblink: https://www.cdc.gov/fungal/diseases/candidiasis/thrush/index.html
Watch Videos To Learn More