
What is a Scabies infection?
Scabies is a skin infestation with the human parasitic itch mite called Sarcoptes scabiei var. hominis. (Citations: 1, 2) There are two types of scabies: classic scabies and crusted (Norwegian) scabies. The crusted (Norwegian) scabies occurs in people with a weakened immune system, or when a person is infected with the new medicine resistant form of scabies. (Citation: 2) The scabies mite digs burrows in the upper layer of the skin where it can live throughout all stages of its life cycle. (Citation: 3)
There are four stages in the life cycle of the scabies mite: egg, larva, nymph and adult. The life cycle of the human scabies mite shows clearly that the mite prefers the human host to survive, although modern DNA sequencing is showing that the human scabies mite potentially has other hosts and can mate and lays its eggs in the human skin as well as other mammals. The eggs are 0.10-0.15 mm in length, and the female adults are 0.30-0.45 mm long, with the male adults being a bit smaller. (Citation: 3)
The WHO declared scabies a be a neglected tropical disease (NTD) in 2017, although it also occurs in non-tropical countries so do not let the name fool you. (Citation: 4) There are also other forms of Sarcoptes scabiei mites that were once thought only to infect animals. However, recent DNA testing of scabies that infects humans has proven that humans can carry a wider variety of Sarcoptes scabiei varieties than previously believed.
Dr. Fischer said her team compared DNA sequences from human scabies mites with those from domestic pigs, which commonly have scabies. “One of the unexpected things we found was that one patient was infected with mites that were genetically more similar to pig mites than to human mites,” she said. “This suggests it may be possible for certain animal strains of mites to infect humans, which we did not previously know was possible. If subsequent studies confirm this finding, it could have major implications for disease control programs.” (Citation: 15)
How common is a Scabies infection?
WHO estimates that there at any time at least 130 million people infested by Scabies worldwide. This means the potential for a person to become infected with scabies in their lifetime is very high, with the actual number of people who have been affected and successfully treating the only limiting factor to this being a global epidemic of disastrous magnitude. Scabies infestations occur in every country in the world to people from every socio-economic background.
Scabies mites are becoming resistant to traditional treatment methods, and the rate of infection is increasing globally. Most of the focus of scabies is placed on developing countries and special groups (institutionalized and vulnerable people) in developed countries. When the reality is scabies mites can and do infect anyone without discrimination. Scabies is one of the most common skin conditions globally, with a prevalence between 0.3% and 46%, with the highest rates in poor tropical areas especially in overcrowded conditions. (Citation: 5)
Is a Scabies infection contagious?
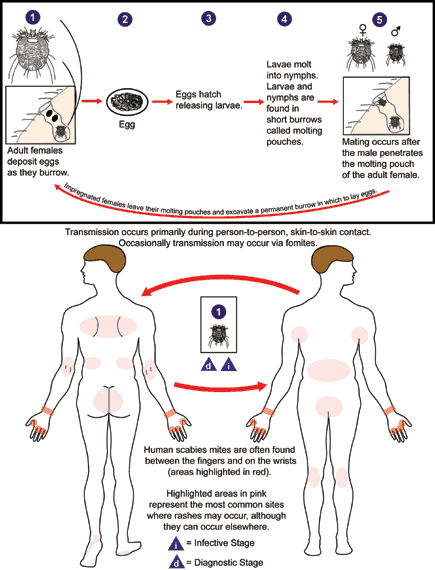
Transmission of scabies occurs through the transfer of pregnant female mites. One of the ways for this transmission to happen is by person-to-person skin contact for a prolonged period of time although even brief contact might also be sufficient for a single scabies mite to transfer from one person to another. Transmission can also occur through contact with personal items like clothing or bedding which are infested with the scabies mite.
In the past, many doctors believe an infected person is no longer contagious within 24 hours after an effective treatment, but scabies mites are now becoming resistant to traditional treatments. Even after the use of scabicides, scabies can still infect a person and infect others. Longer and stronger treatment is needed in these types of infestations, and these cases are becoming more and more common. (Citation: 5)
An infected person can be without symptoms up to 6 weeks or longer, especially if this is their first scabies infection. Even if they are without symptoms, they are still contagious and thus can spread the disease. People with crusted scabies are much more infectious than people with classic scabies because their skin contains a much more significant number of mites (up to 2 million). (Citation: 6)
What are signs and symptoms of a Scabies infection?
Symptoms typically begin to occur in a first scabies infection within 2-6 weeks and after 1-4 days if the person had a scabies infection before. An allergic reaction to the proteins and feces of the mite(s) results in severe itching (pruritus), especially at night, and a pimple-like (popular) rash. Tiny burrows can sometimes be seen on the skin. Human scabies mites are often found on the Scalp, Face, ears, wrist and between the fingers. Other common sites are elbows, armpits, genital area, chest, waist, buttocks, knees, feet and shoulder blades. Common sites in young children are palms, soles, head, face and neck. (Citations: 2, 3, 6, 7) Basically, any area of skin on the human body can be a breeding ground for scabies.
Crusted (Norwegian) scabies occurs in people with less immunity, but also in the elderly and in people who cannot itch or scratch. In this type of scabies, there are crusts and blisters (vesicles) all over the skin that contain many mites. Preferred locations are the hands, feet and scalp but it quickly becomes widespread. Scratch or itch marks might be absent. People with crusted scabies are very contagious because their skin contains many mites. (Citations: 2, 6)

How to diagnose a Scabies infection in humans?
Diagnosing scabies infections is usually made on the clinical presentation of the intense itching, the rash and the burrows. This can be complemented by finding mites, but finding and examining mites is not needed to make a diagnosis of scabies as the symptoms alone can show high potential for a person being infected with scabies.
It should be noted that an otherwise healthy person infected with scabies might only have as few as 10-15 mites on the body. However, even a person infected with several hundred mites can present with little noticeable symptoms. Mites can potentially be found on any part of the body and are not limited to the wrist and between the fingers as was once believed. (Citation: 3) A mite can be removed at the end of its burrow with the tip of a needle and examined under the microscope, although this is very difficult to do and almost never done successfully in real-world circumstances as finding an easily removable specimen is not very easy. Alternatively, when a person has crusted scabies, a skin scraping can be examined under the microscope for mites, mite eggs or mite feces (scybala). (Citations: 2, 8, 9)
What Is the treatment for a Scabies infection?
Treatment for scabies is usually with a topical application of a scabies killing agent (scabicide), for example permethrin, malathion, benzyl benzoate, Sulphur ointment or lindane. Oral Ivermectin is also used as treatment.
It is essential to treat the whole household at the same time to prevent re-infection. (Citations: 2, 3, 10) Also, personal items like bedding and clothing should be washed and dried at high temperature or be kept in plastic bags for several days. Putting items overnight in a freezer can also help eliminate mites on items (Citation: 4) Mites usually do not survive more than 2-3 days away from the human body, although it is possible. (Citation: 4)
A recent Cochrane review concluded that topical permethrin combined with oral ivermectin simultaneously appears to be the most preferred treatment. This study also stated that more research is needed on the effectiveness of malathion, and on the management of scabies in larger settings (institutions, communities). (Citation: 11) Crusted (Norwegian) scabies needs to be treated rapidly and aggressively to prevent outbreaks. (Citation: 4)
What are complications from Scabies infections?
The main complication is a secondary bacterial skin infection (impetigo), which can be treated with antibiotics. (Citation: 3) The impetigo can cause problems in other parts of the body: it can spread to the bloodstream, kidney and heart resulting in sepsis, renal disease and rheumatic heart disease. (Citation: 12) The renal disease is usually a post-streptococcal glomerular nephritis. (Citation: 6)
What are preventive measures against Scabies?
The primary prevention measure against scabies is avoiding direct skin-to-skin contact with an infected person. Prolonged skin contact increases the likelihood to transmit classic scabies, while for crusted (Norwegian) scabies even very brief skin contact can easily be sufficient. Scabies can also be transmitted through contact with personal items that the infected person wore or used close to the skin like bedding and clothing. Also sleeping in the bed of an infected individual, even when no one else is sleeping in it, can cause infection. Many people have reported getting infected with scabies after staying in a hotel bed, also a five-star hotel. (Citation: 5)
Evidence on prophylaxis is lacking, for example, a recent Cochrane review did not find any randomized controlled studies on prophylaxis (preventative medication or personal hygiene advice) of scabies in people who had been in close contact with a scabies case. (Citation: 13) The International Alliance for the Control of Scabies (IACS) (Citation: 14) is currently looking into ways for population control of Scabies, for example through mass drug administration (MDA) of ivermectin or a topical scabicide. Several MDA studies are currently underway to look into the possibilities of using Moxidectin as a new form of scabies treatment. (Citation: 3)
Resources
- Centers for Disease Control and Prevention. Accessed online 5th October 2017. Weblink: https://www.cdc.gov/parasites/scabies/gen_info/faqs.html
- Merck Manual Professional Version. Accessed online 5th October 2017. Weblink: http://www.merckmanuals.com/professional/dermatologic-disorders/parasitic-skin-infections/scabies
- Centers for Disease Control and Prevention. Accessed online 5th October 2017. Weblink: https://www.cdc.gov/parasites/scabies/biology.html
- International Alliance for Control of Scabies. News article. Accessed online 5th October 2017. Weblink: http://www.controlscabies.org/news/who-adds-scabies-ntd-list/
- World Health Organization. Accessed online 5th October 2017. Weblink: http://www.who.int/lymphatic_filariasis/epidemiology/scabies/en/
- Centers for Disease Control and Prevention. Accessed online 5th October 2017. Weblink: https://www.cdc.gov/parasites/scabies/disease.html
- Mayo Clinic. Accessed online 5th October 2017. Weblink: http://www.mayoclinic.org/diseases-conditions/scabies/basics/symptoms/con-20023488
- Centers for Disease Control and Prevention. Accessed online 5th October 2017. Weblink: https://www.cdc.gov/parasites/scabies/diagnosis.html
- Centers for Disease Control and Prevention. Accessed online 5th October 2017. Weblink: https://www.cdc.gov/dpdx/scabies/index.html . Go to tabs: Image Gallery AND Laboratory Diagnosis
- Centers for Disease Control and Prevention. Accessed online 5th October 2017. Weblink: https://www.cdc.gov/parasites/scabies/prevent.html
- Cochrane Reviews. Accessed online 5th October 2017. Weblink: http://www.cochrane.org/CD000320/INFECTN_interventions-for-treating-scabies
- Romani L and others. Prevalence of scabies and impetigo worldwide: A systematic review. Lancet Infectious Diseases 2015 August; 15(8): 960-7. doi: 10.1016/S1473-3099(15)00132-2. Epub 2015 Jun 15. Weblink: https://www.ncbi.nlm.nih.gov/pubmed/26088526
- Cochrane Reviews. Accessed online 5th October 2017. Weblink: http://www.cochrane.org/CD009943/OCCHEALTH_interventions-for-preventing-the-spread-of-infestation-in-close-contacts-of-people-with-scabies
- International Alliance for Control of Scabies. Agency website. Accessed online 5th October 2017. Weblink: http://www.controlscabies.org/
- Walter and Eliza Hall Institute Accessed online 5th October 2017. https://www.wehi.edu.au/news/gene-technology-help-healthy-skin-aboriginal-australians

