Whipworm in humans (Trichuriasis)

What is a Whipworm infection?
Whipworms get their name because their shape resembles a whip.
Whipworm is the common name of the parasitic roundworm (nematode) Trichuris trichura. The medical term for a whipworm infection is trichuriasis. (Citation: 1) Whipworm infections are one of the most common soil-transmitted helminths (parasitic worms) that infect humans. Trichuriasis often also occurs together with other parasitic worm infections like Ascariasis and hookworm infections. (Citation: 3) Adult whipworms are about 3-5 cm long. T. trichura was first discovered in 1740, while trichura eggs have been found at archeological sites that date back much further. Cases of whipworms infecting human’s dates back to at least Ancient-Roman times. (Citations: 4, 5, 6)
How common are Whipworm infections?
It is estimated that between 604 and 795 million people in the world have whipworm infection. Whipworm infections are common in warm and humid climates, especially where sanitation and hygiene are poor. Whipworm infections are more common during the warmer months of the year, and in temperate climates around the world. (Citations: 7,8)
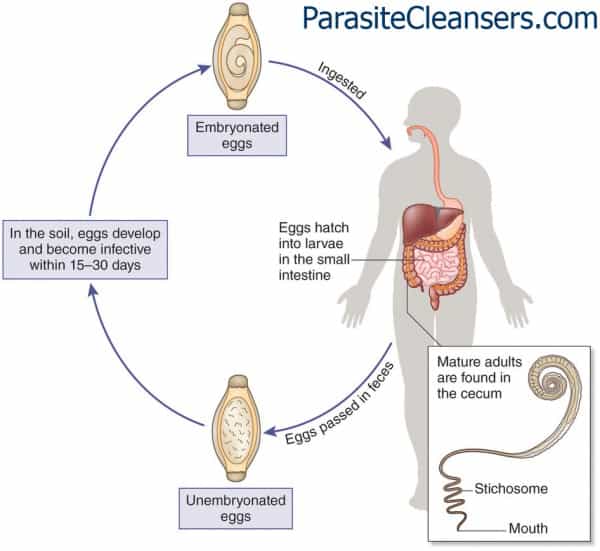
Adult whipworms can survive in the human intestines for at least one year. The female whipworms produce un-embryonated eggs that are deposited into the feces within the intestine tract. The eggs will develop further and potentially mature if they are able to reach the soil. This is made possible when human feces is used as a fertilizer or if people defecate out in the open directly on the soil. Once in the soil, the development of the eggs goes through several stages. Ultimately, it takes 15-30 days to reach the mature (embryonated) stage. The whipworm eggs can become ingested after clinging to hands and making their way into a person’s mouth. After ingestion of the eggs by soil-contaminated hands or food, the eggs hatch in the small intestine where they develop into larvae. Once the larvae mature, they can easily live by attaching to the mucosa of the colon. Female worms in the colon can produce as many as 20,000 eggs per day, and they cycle continues. (Citation: 2)
Is a Whipworm infection contagious?
Only the fully mature eggs of the whipworm are considered infectious. Ingestion of the mature T. trichura eggs from contaminated soil will result in a whipworm infection in humans. This happens when soil-contaminated vegetables or fruits which have not been carefully peeled, washed or cooked are eaten. Infection also occurs when hands or fingers that contain infected soil are put into the mouth. (Citation: 8)
Direct person-to-person infection from eggs moving from one person to another, like in pinworm infections, is not possible in trichuriasis because the eggs first must mature outside the body in soil.
CDC has a nice illustration of the Trichuris lifecycle. (Citation: 2)
Signs and symptoms of a Whipworm infection
Light whipworm infections are often without symptoms. Symptoms of heavy whipworm infections can include abdominal pain, loss of appetite, nausea, vomiting, diarrhea, dysentery (bloody diarrhea), weight loss, anemia and rectal prolapse. In rectal prolapse the rectal mucosa or the entire rectal wall can protrude through the anus. Besides the extreme discomfort, this can also lead to constipation. (Citations: 1, 9)

How to diagnose a Whipworm infection in humans?
The diagnosis of trichuriasis is made through a microscopic examination of the stool to determine the presence of whipworm eggs. Whipworm eggs have a well-defined and distinguishable appearance. Whipworm eggs are barrel-shaped or lemon-shaped with a thick-shell and the presence of polar “plugs” at both ends. In case of mild infections, a concentration method like Kato-Katz might be needed for the stool examination. (Citations: 10, 11, 1) Sometimes Trichuris worms are accidentally found during endoscopic investigations of the anus, rectum or colon (anoscopy, proctoscopy or colonoscopy). (Citation: 1)
What Is the treatment for a Whipworm infection?
One treatment for a whipworm infection is with oral pharma medications. The options most prescribed include are Mebendazole (3 days), Albendazole (3 days) and Ivermectin (3 days). Patients that have a co-infection with Loa loa can get severe reactions to the Ivermectin. Therefore, if Ivermectin is planned as a treatment option, patients that have been to Central Africa should be tested for Loa Loa. (Citation: 1)
What are complications of Whipworm infections?
Complications of whipworm infections mostly occur in cases where there is a severe infestation (many worms). The most common complications are rectal prolapse, dysentery, anemia, vitamin deficiency. In severe prolonged infections in children malnutrition can result in growth retardation and impaired cognitive development. (Citations: 13,14)
What are preventive measures against Whipworm?
Preventive measures for whipworm infections include three main approaches:
- Health education to prevent infecting others and re-infection of self.
- Improved sanitation practices to reduce contamination of soil with whipworm eggs.
- Periodic deworming of the household to eliminate worms in people.
(Citations: 15,3)
Health education is vital in whipworm infection prevention. Preventing ingestion of eggs from hands or food that contain infected soil will break the transmission cycle, as the human is the only known host for T. trichura. This means that handwashing with soap and water before preparing, handling or eating food as well as proper washing, peeling and cooking of food are essential measures. Other measures include not defecating outside in the soil but only in a latrine or toilet which utilize safe and effective feces disposal systems. (Citation: 16)
Where hygiene is difficult to maintain, for example in developing countries, regular mass campaigns with Mebendazole (single dose) has been used to control trichuriasis and other parasitic worm infections. (Citation: 1) Current scientific research has focused on identifying the ideal environmental conditions for egg maturation. The goal is to identify critical prevention and control activities within specific high-risk areas. (Citation: 17)
References
- Merck Manual Professional Version. Accessed online 21st September 2017. Weblink: http://www.merckmanuals.com/professional/infectious-diseases/nematodes-roundworms/trichuriasis
- Centers for Disease Control and Prevention. Accessed online 21st September 2017. Weblink: https://www.cdc.gov/parasites/whipworm/biology.html
- World Health Organization. Accessed online 21st September 2017. Weblink: http://www.who.int/mediacentre/factsheets/fs366/en/
- Accessed online 21st September 2017. Weblink: http://emedicine.medscape.com/article/788570-overview
- Stanford University. Accessed online 21st September 2017. Weblink: https://web.stanford.edu/group/parasites/ParaSites2005/Trichuris/index.htm
- Dufour and others. A first case of human trichuriasis from a Roman lead coffin in France. Korean J Parasitol. 2016 Oct; 54(5): 625–629. Published online 2016 Oct 31. doi: 3347/kjp.2016.54.5.625. Weblink: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5127534/
- Centers for Disease Control and Prevention. Accessed online 21st September 2017. Weblink: https://www.cdc.gov/parasites/whipworm/
- Centers for Disease Control and Prevention. Accessed online 21st September 2017. Weblink: https://www.cdc.gov/parasites/whipworm/gen_info/faqs.html
- Accessed online 21st September 2017. Weblink: http://www.healthline.com/health/whipworm-infection#symptoms2
- Centers for Disease Control and Prevention. Accessed online 21st September 2017. Weblink: https://www.cdc.gov/parasites/whipworm/diagnosis.html
- Centers for Disease Control and Prevention. Accessed online 21st September 2017. Weblink: https://www.cdc.gov/dpdx/trichuriasis/index.html (tabs: Image Gallery and Laboratory Diagnosis)
- Centers for Disease Control and Prevention. Accessed online 21st September 2017. Weblink: https://www.cdc.gov/globalhealth/ntd/diseases/whipworm_burden.html
- Accessed online 21st September 2017. Weblink: http://emedicine.medscape.com/article/788570-followup?pa=QXM1sfONOtEPdqDXoIwOQS4w4mnx%2Fvsb1jmMzcyDbnASYHhim7CQ85da85f1ddEjEpC0%2FbDJCwARAavA5XkKAnK0iO93RZdqhp7TL4xDMLE%3D#e4
- Centers for Disease Control and Prevention. Accessed online 21st September 2017. Weblink: https://www.cdc.gov/parasites/whipworm/disease.html
- Ziegelbauer K, Speich B, Mausezahl D, Bos R, Keiser J, Utzinger J. Effect of sanitation on soil-transmitted helminth infection: systematic review and meta-analysis. PLOS Medicine 2012; 9(1):e1001162. Weblink: https://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0051379/
- Centers for Disease Control and Prevention. Accessed online 21st September 2017. Weblink: https://www.cdc.gov/parasites/whipworm/prevent.html
- Manz and others. Trichuris trichiura infection and its relation to environmental factors in Mbeya region, Tanzania: A cross-sectional, population-based study. Published: April 6, 2017. https://doi.org/10.1371/journal.pone.0175137. Weblink: http://journals.plos.org/plosone/article?id=10.1371/journal.pone.0175137
Watch Videos To Learn More

