Pinworm (Enterobiasis) Threadworm symptoms and treatment in humans
What is a Pinworm infection?
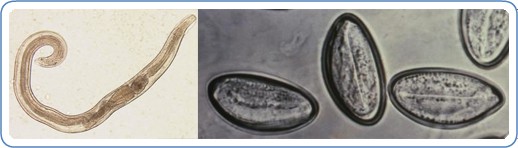
Pinworm infection is caused by a roundworm (or nematode) called Enterobius vermicularis. The medical term for pinworm infection is Enterobiasis. (Citations: 1, 2) CDC has made a nice graphic presentation of the Enterobius lifecycle. (Citation: 3) Female pinworms are small (5-13 millimeter), thin and white worms (the males are 2-5 mm). (Citations: 4, 12) Pinworm eggs are very tiny and only visible under a microscope. Pinworm infections have been reported from as far back as 10,000 years ago in the Americas in a recent (2016) study. (Citation: 5)
How common are Pinworm infections?
Enterobiasis is one of the most common roundworm infection in the world. It is more frequent in (pre-)school children and their caretakers, in crowded situations (e.g. in institutions, camps) and in temperate climates. Enterobiasis is the most common worm infection in the United States, where there are an estimated 40 million people infected with pinworm. (Citation: 6)
Is a Pinworm infection contagious?
The only host for pinworm is the human. A person gets infected through ingestion of pinworm eggs. These microscopic eggs can transfer from contaminated surfaces: hands (own or others), toys, bed linen, clothing, toilet seats and other public areas to one’s hands or mouth. It is even possible to breathe in pinworm eggs because they are so small. After ingestion, it takes 1-2 months to form adult worms in the small intestine, which then migrate to the colon to lay eggs around the anus at night. Reinfection can occur from ‘own’ eggs or eggs from another person. A person is contagious as long as that person has adult worms living in his/her body. Eggs in the environment (outside the body) can survive up to 3 weeks. (Citations: 7, 3, 12)
What are the signs and symptoms of Pinworm infections?
Enterobiasis infections are often asymptomatic. (Citation: 8) The most common symptom is itching in the anal area. Other reported symptoms are teeth grinding, sleeplessness and abdominal pain. (Citation: 9) There might also be complaints from (rare) complications like a bacterial infection of the scratch wounds and infection of other organs, like the female genital organs, by migrating worms (see below on complications). (Citation: 10)
How to diagnose Pinworm infections in humans?
As pinworm eggs and worms are only available in minimal amounts in the stool, it is not advisable to investigate stool samples. There are unfortunately no serologic (blood) tests available for enterobiasis. There are however three simple ways to look for the worms or eggs (Citations: 7, 11, 12):
- Looking for the thin white female worms (size 5-13 millimeter) in the perianal area (preferably 2-3 hours after the person is asleep)
- Using sticky transparent tape to collect possible eggs from the perianal skin (preferably when the person just wakes up from sleep, on three consecutive days). The tape can be examined under the microscope.
- Collection of scrapings from under the fingernails for microscopic examination for eggs
Sometimes eggs are also found, as unexpected findings, in urine or vaginal smears.

What is the treatment for Pinworm infections in humans?
Treatment for pinworm infection is with oral medication: albendazole, mebendazole or pyrantel palmoate. The last medication is available without prescription in the USA. (Citation: 12) The medication is given in a single dose, followed by another single dose after two weeks. The second single dose is needed because of possible re-infection by adult worms that hatched from eggs that were not killed by the first treatment. (Citation: 13) Mass treatment can be considered in institutions and households were more than one person is infected. (Citation: 14)
Are there complications from Pinworm infections?
Complications in pinworm infections are not common. Sometimes there is a bacterial superinfection of the perianal scratch wounds. Rarely the worms migrate to other areas of the body, for example, the female genitals. (Citation: 15) This can result in for example vaginitis and endometritis (infection of the uterus lining). (Citation: 16) Another rare complication because of worm migration is appendicitis. (Citation: 17, 18)
Preventive measures against Pinworm infections
As humans are the only host of pinworm, the prevention of both spread and re-infection is focused on personal and household hygiene. The best measure is handwashing (with soap and warm water) by both infected and not-infected persons, especially after going to the toilet, after changing diapers and before preparing and eating food. Infected persons should bathe every morning to remove the eggs of the skin. Showers are preferred as this prevents contamination of bath water with pinworm eggs. Of course, co-bathing should be avoided also.
Infected persons should cut their fingernails short and should avoid biting nails and scratching in the perianal area. All bed/underclothes and bed linens of infected individuals should be washed with hot water: they should be taken in the morning and carefully handled (to avoid spreading the microscopic eggs) before putting them in the washer. If available, they can be dried in a hot dryer after washing to kill any surviving eggs. Mass drug application has been used in institutions, schools and day care centers for enterobiasis outbreaks.
Vacuuming can also assist in eliminating eggs from the environment. (Citation: 19, 12)
References
- Centers for Disease Control and Prevention. Accessed online 18th September 2017. Weblink: https://www.cdc.gov/parasites/pinworm/
- Accessed online 19th September 2017. Weblink: https://www.uptodate.com/contents/enterobiasis-pinworm-and-trichuriasis-whipworm
- Centers for Disease Control and Prevention. Accessed online 18th September 2017. Weblink: https://www.cdc.gov/dpdx/enterobiasis/index.html
- Mayo Clinic. Accessed online 19th September 2017. Weblink: http://www.mayoclinic.org/diseases-conditions/pinworm/basics/definition/con-20027072
- Reinhard and others. “Temporal and spatial distribution of Enterobius Vermicularis (Nematoda: Oxyuridae) in the prehistoric Americas”. The Korean Journal of Parasitology. 2016 October; 54(5): 591-603. Published online 2016 Oct 31. doi: 3347/kjp.2016.54.5.591. Weblink: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5127543/
- Centers for Disease Control and Prevention. Accessed online 18th September 2017. Weblink: https://www.cdc.gov/dpdx/enterobiasis/index.html
- Centers for Disease Control and Prevention. Accessed online 19th September 2017. Weblink: https://www.cdc.gov/parasites/pinworm/epi.html
- Centers for Disease Control and Prevention. Accessed online 19th September 2017. Weblink: https://www.cdc.gov/parasites/pinworm/diagnosis.html
- Tehrani and others in “The correlation between intestinal parasitic infections and bruxism among 3-6 year-old children in Isfahan”. Dental Research Journal. 2010 Summer-Autumn; 7(2): 51-55. Weblink: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3177368/
- Centers for Disease Control and Prevention. Accessed online 19th September 2017. Weblink: https://www.cdc.gov/parasites/pinworm/disease.html
- Mayo Clinic. Accessed online 19th September 2017. Weblink: http://www.mayoclinic.org/diseases-conditions/pinworm/basics/tests-diagnosis/con-20027072
- Merck Manual Professional Version. Accessed online 19th September 2017. Weblink: http://www.merckmanuals.com/professional/infectious-diseases/nematodes-roundworms/pinworm-infestation
- Centers for Disease Control and Prevention. Accessed online 18th September 2017. Weblink: https://www.cdc.gov/parasites/pinworm/health_professionals/index.html
- Centers for Disease Control and Prevention. Accessed online 19th September 2017. Weblink: https://www.cdc.gov/parasites/pinworm/treatment.html
- Powel and others in “Enterobius vermicularis infection of the ovary”. BMJ Case Reports. 2013; 2013: bcr2013201146. Published online 2013 Oct 31. doi: 1136/bcr-2013-201146/ Weblink: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3822223/
- Mayo Clinic. Accessed online 19t September 2017.Weblink: http://www.mayoclinic.org/diseases-conditions/pinworm/basics/complications/con-20027072
- Enterobiasis: threadworm infection presenting as acute appendicitis in a 13-year-old girl. BMJ Case Reports. 2015; 2015: bcr2014208543.Published online 2015 Jan 14. doi: 10.1136/bcr-2014-208543. Weblink: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4307057/
- Altun and others in “Parasitic infestation in appendicitis. A retrospective analysis of 660 patients and brief literature review”. Saudi Medical Journal. 2017 March: 38(3): 314-318. doi: 15537/smj.2017.3.18061. Weblink: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5387911/
- Centers for Disease Control and Prevention. Accessed online 19th September 2017. Weblink: https://www.cdc.gov/parasites/pinworm/prevent.html
Watch Videos To Learn More